Degenerative Disc Disease (DDD) is a common yet challenging condition that significantly affects a patient’s mobility and quality of life. As discs between the vertebrae lose their flexibility and cushioning ability, patients experience pain, stiffness and sometimes nerve damage that impacts daily activities. Dr. Larry Davidson, a leader in spinal surgery, recognizes that spinal fusion surgery has long been a treatment option for stabilizing the spine and alleviating these symptoms, yet traditional approaches have limitations, especially in terms of precision and durability.
Artificial Intelligence (AI) is now transforming the treatment of DDD, enhancing spinal fusion surgery outcomes by making them more precise, personalized and effective. AI’s integration into spinal fusion procedures offers new possibilities for treating degenerative conditions like DDD, providing patients with greater hope for improved quality of life and mobility.
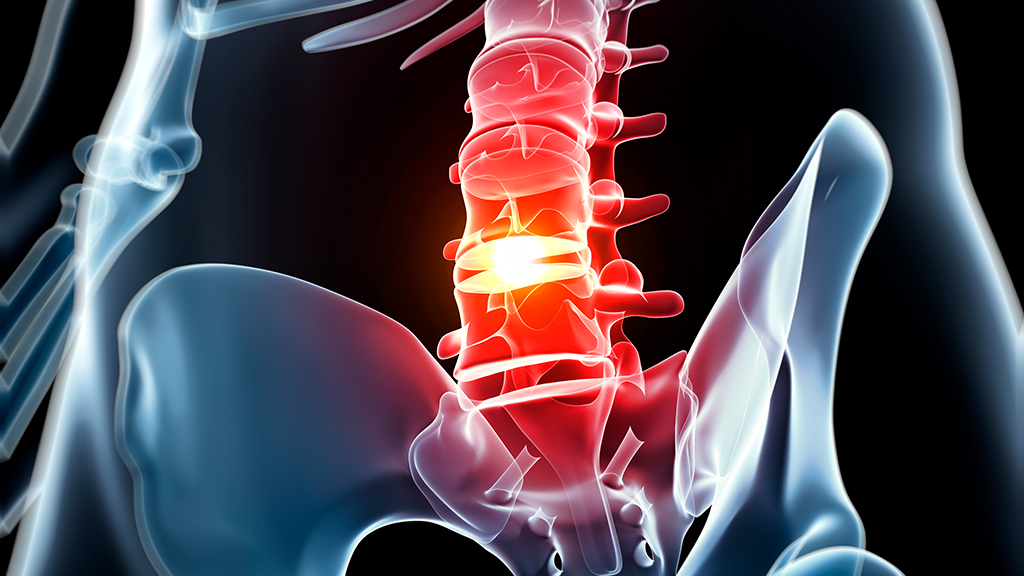
Understanding Degenerative Disc Disease and Spinal Fusion
Degenerative disc disease progresses as the spinal discs between vertebrae wear down due to age, injury or genetic predispositions. Healthy discs act as shock absorbers, protecting vertebrae and nerves from strain. However, in DDD, the loss of flexibility in these discs causes pain and can lead to nerve impingement, reduced mobility and chronic discomfort. For many DDD patients, spinal fusion surgery is recommended to relieve these symptoms and provide spinal stability. The procedure joins two or more vertebrae, stabilizing the spine but sometimes reducing flexibility, so precision in planning and execution is vital to achieving long-term success.
Traditional spinal fusion has served as an effective solution for many, but there are challenges, such as ensuring that the fusion remains stable and that the patient maintains optimal function over time. AI is helping to address these issues by enhancing how DDD is treated through more refined, data-driven surgical planning and personalized recovery support.
AI’s Role in Preoperative Planning
AI significantly enhances preoperative planning for DDD patients by analyzing imaging, patient history and genetic data to understand each patient’s specific spinal health. This allows surgeons to design personalized surgical strategies tailored to individual needs.
AI also simulates different surgical approaches, helping surgeons choose the most effective hardware placements for stabilization and pain relief. This thorough planning improves outcomes by addressing the unique challenges of DDD, increasing the precision and effectiveness of spinal fusion procedures.
Enhancing Surgical Precision with AI
During spinal fusion surgery, AI provides real-time feedback and guidance, significantly enhancing surgical precision. AI-powered systems monitor the surgeon’s movements and can assist in aligning screws, rods and other hardware with extreme accuracy. In spinal fusion, even a slight misalignment can lead to complications such as nerve damage or hardware failure, so the precision that AI offers is especially valuable.
AI’s ability to deliver intraoperative guidance helps reduce errors and improve patient outcomes. If AI detects any deviations from the planned surgical path, it can alert the surgeon immediately, allowing adjustments to be made on the spot. This dynamic support ensures that DDD patients receive a highly accurate spinal fusion, reducing the likelihood of post-surgical complications. The combination of AI-guided preoperative planning and intraoperative assistance allows for a more precise procedure, ultimately improving the quality of spinal fusion for those suffering from degenerative disc disease.
Improving Long-Term Outcomes for DDD Patients
Achieving long-term stability and pain relief is a primary goal of spinal fusion surgery for DDD patients, and AI plays a crucial role in meeting this goal. By analyzing the patient’s anatomy, condition and lifestyle, AI can predict how the fusion will hold up over time. These predictions allow surgeons to select techniques and hardware that best support the patient’s spinal health, reducing the likelihood of complications or hardware failure in the years following surgery.
AI provides insights into the unique demands each patient’s lifestyle places on their spine, helping surgeons make informed choices about stabilization techniques and hardware positioning. By predicting how the spine will respond to daily activities post-surgery, AI aids in tailoring each fusion to provide stability and function. This personalization ensures that patients experience long-term relief from DDD symptoms, improving their mobility and quality of life in the years following surgery.
Monitoring Post-Surgical Recovery with AI
AI continues to support DDD patients throughout recovery by using wearable technology and apps to monitor key metrics like mobility, pain and spinal stability. This real-time tracking provides healthcare providers with insights to promptly address issues, such as inflammation or hardware misalignment, before they escalate.
AI also personalizes rehabilitation by analyzing recovery progress and adjusting exercise intensity as needed. This tailored approach ensures each patient’s recovery plan aligns with their pace, enhancing outcomes and promoting a smoother, more effective recovery.
Enhancing Patient Engagement and Accountability
AI-powered tools and wearable devices not only monitor recovery but also enhance patient engagement by providing real-time feedback on progress. Patients can track their mobility, pain levels and other indicators of healing, helping them stay informed about their recovery journey. For DDD patients, this engagement provides a sense of control over their recovery and fosters a greater commitment to following their rehabilitation plan consistently.
AI-driven apps can also provide reminders for physical therapy, medication and follow-up appointments, helping patients adhere to their recovery schedules. This accountability is critical for maintaining consistent rehabilitation, which is essential for optimal results after spinal fusion. By actively involving patients in their own recovery, AI encourages habits that promote healing and reduce the risk of setbacks, making the recovery process more effective and engaging.
The Future of AI in Treating Degenerative Disc Disease
As AI advances, its role in spinal fusion for DDD patients will expand. Future improvements may include more refined preoperative simulations, greater use of genetic data and biomechanical modeling to enhance personalized care.
Integration with wearable technology could offer deeper insights, tracking metrics like bone density and muscle strength to ensure stable, long-term recovery. These advancements will make AI an essential tool for managing DDD, helping patients achieve lasting relief and improved mobility.
AI is revolutionizing the treatment of degenerative disc disease through its integration into spinal fusion surgery. Dr. Larry Davidson remarks, “AI will provide us with the ability to have a total and comprehensive understanding of a patient’s medical history, and what sort of spinal interventions would be considered as best practices.” It will allow surgeons to quickly review and summarize existing medical literature for specific patients with unique conditions, ensuring they can apply the most optimal treatment options for everyone.
Beyond diagnostics, AI is making significant strides in preoperative planning, surgical precision and recovery monitoring. These innovations bring a more personalized, data-driven approach to treatment, improving long-term outcomes for DDD patients. By enhancing mobility, expediting recovery and restoring quality of life, AI is offering renewed hope to individuals facing this challenging condition. As its role continues to expand, AI will become an essential element in developing tailored and effective solutions for DDD management.